
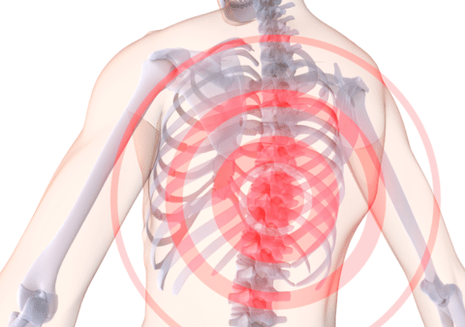
Many people aged 30-35 complain about back pain.The cause of these pains may be the disease of the spine.Osteochondrosis is a disease that occurs in middle -aged people, but more often it is detected in patients after 40 years.
Osteochondrosis - what is this disease, and what is its danger?
This term means a dystrophic process of cartilage and subject bone tissue.In modern medical practice, osteochondrosis is called a degenerative-dystrophic disease of the spine and intervertebral discs that play the role of the shock absorber.The danger of the disease is that the affected disc is almost impossible to restore, and without proper treatment, disability is possible.
Osteochondrosis is a common disease?Statistics are not happy.About 85% of the population in the world suffers from this disease.
This disease is the most common form among all diseases that affect the spine.And according to prevalence, it is immediately after diseases of the cardiovascular system.
The essence of the disease
So, osteochondrosis - what is it?This is a chronic disease that affects the joints, most often the spine.
The spinal column consists of 24 vertebrae.Between the two vertebrae is a disk, the purpose of which is the softening and depreciation of loads.
In normal condition, the disk is quite elastic and can withstand significant loads.In the center of the disk there is a pulp nucleus with a lot of water.For some reason, the core loses its hydrophilic properties.
As a result, the disk delays, decreases in height and deform.In the later stages, bone tissue growth occurs with the formation of growths - osteophytes that compress the peripheral nerves and spinal cord.This is what is osteochondrosis of the spine.
The causes of pathology
Despite the fact that osteochondrosis is a fairly common disease, the reasons why pathology develops is not completely established.

The main factors are considered:
- excessive load on the spine;
- injuries;
- professional harmfulness - weight lifting or prolonged work in an uncomfortable, motionless pose;
- excess body weight;
- heredity;
- violation of posture.
Osteochondrosis develops to one degree or another in almost all people of the elderly and is one of the processes of aging of the body.
Stages, forms and symptoms of the development of the disease
Experts distinguish 4 stages of the disease:
- 1st stage- moving the nucleus of the disk to the edge;
- Stage 2- the occurrence of cracks in the wheels of the cartilage and the instability of the vertebral section;
- Stage 3- a complete rupture of the disk with the loss of the nucleus in the stem of the spine, while the roots of the spinal cord are possible;
- 4th stage- Rough changes not only in the intervertebral disk, but also in the surrounding fabrics.
The main symptom of the disease is pain.It can be acute with high intensity or dumb, moderate manifestation.
In addition to pain, there are:
- painful tension of the back muscles;
- numbness of the skin on the arms and legs;
- limitation of the volume of movements;
- weakness in the muscles of the limbs;
- thinning of the arms and legs;
- Sudden dizziness.
These are general manifestations for all forms of pathology.Depending on the spine in which changes are localized, three forms of the disease with characteristic symptoms are distinguished.
Table No. 1.Forms of osteochondrosis and their inherent symptoms:
| Form of the disease | Symptoms |
| Osteochondrosis in the neck | Changes in this department lead to pushing blood vessels and impaired microcirculation.For this reason, a person has constant dizziness.Sometimes this leads to fainting.There are noise in the ears and flickering of colored spots in front of the eyes. |
| Osteochondrosis in thoracic vertebrae | With this form of the disease, acute chest pain is observed.The disease can cause the progression of intercostal neuralgia and aggravate the course of heart pathologies. |
| Osteochondrosis in the lumbar region | The pathology in the lower back is manifested by pain in the gluteal region, a decrease in the tone of the IKR.A complication can be radiculite, which is accompanied by pain spreading throughout the leg. |
Due to the pathology of the vertebral discs, a large number of disorders in the body occurs: pinching of nerves, swelling, circulatory violation, and fibrosis of the surrounding tissues.These changes cause a variety of symptoms, which complicates the diagnosis and prescribe the appropriate treatment without a carefully examination.
Clinical manifestations
The symptoms of the disease depends on where the lesion is mainly located.In the sections below, we consider the signs characteristic of each variety of the disease.
The cervical department

The main symptoms of damage to the cervical spine include:
- discomfort, soreness in the neck and shoulders;
- muscle hypotonus;
- increased sweating;
- numbness of the fingers;
- violation of coordination of movements;
- headaches, dizziness;
- Problems with hearing and vision;
- Hypertension.
With the progression of the disease and damage to the nearby arteries and nerves, one of the following syndromes can develop:
- vertebral artery;
- cardiac;
- hypertension;
- root;
- cervical migraine.
Violation of blood circulation in the vertebral artery and this hypoxia of brain tissues are the dangerous consequences of osteochondrosis.
This syndrome manifests itself:
- system/periodic dizziness;
- weakening of vision;
- partial or complete hearing loss;
- Sometimes - fainting.
Important!Neurological manifestations of osteochondrosis of the spine often have to differentiate with brain atherosclerosis, DEP and other pathologies.
Thoracic region
Compared to other forms of the disease, thoracic osteochondrosis is manifested less pronounced.
Among its symptoms:
- pain in the chest, increasing at night or with prolonged in one position;
- discomfort, a feeling of squeezing between the shoulder blades;
- Strengthening pain during deep breathing.
If the disease is not treated, it will progress, causing damage to the nearby and nerves located nearby.
Signs of the development of complications of osteochondrosis of the spine of this localization can be:
- numbness of the skin in some areas, a feeling of crawling "goosebumps";
- Skin itching, burning;
- cooling of the limbs;
- fragility of nails;
- pronounced dry skin;
- pain along the esophagus and pharynx;
- Disorders of the gastrointestinal tract.
In addition, the chest localization of the disease is characterized by two specific symptoms - Dorsago and Dorsalgia.
Dorsago is a sudden, sharp and very intense chest pain, a “thoracic shift”.It can occur with prolonged in the same position, monotonous work.
Pay attention!During the breastfile, the pain is so severe that patients are afraid to even take an extra inhalation.
Dorsalgia is less intense, but monotonous painful sensations that can last up to 2-3 weeks.They intensify with deep breathing, inclinations.
Lumbar department
Osteochondrosis of the lower part of the spine, namely the lumbar, occupies a leading position on prevalence.

Among his characteristic symptoms:
- dull, more often aching lower back pain, radiating in the leg;
- discomfort, intensifying when changing the position of the body, sneezing, coughing, trying to lift weights;
- constant muscle spasm in the lower back;
- Lights in the lower back;
- impaired sensitivity on the skin of buttocks, hips, legs, feet;
- a feeling of crawling goosebumps on the lower extremities;
- Dry, peeling of the skin.
The sacral department
Osteochondrosis of the sacral spine is extremely rare in an isolated manner and is usually a “continuation” of the lower lumbar damage.
This explains the features of his symptoms:
- lower back pain, as well as in the sealing nerve;
- Sharp "shelters" through the entire leg;
- an unpleasant feeling of discomfort in the back of the thigh;
- numbness of the lower limb;
- Paresis, as well as unstable symptoms of impaired motor activity.
Important!Osteochondrosis of the lower spine can lead to such extremely dangerous complications as impaired blood supply to the spinal cord and compression myelopathy.

Common osteochondrosis
A common form, or osteochondrosis of all parts of the spine is the most severe version of the pathology.Due to the vastness of the defeat, its picture can be extremely diverse and include almost all the symptoms described above.
Diagnostic methods
The appearance of any complaints indicated above requires an appeal to a medical institution: the patient must examine the patient.Diagnosis of osteochondrosis should be complex and very thorough.
The standard instruction includes the following stages:
- Collection of complaints and anamnesis.
- Clinical inspection.
- X -ray examination.
- Modern methods (CT, MRI).
Conducting a conversation with the patient, the doctor should find out:
- which bothers the patient;
- What is the place of the most pronounced unpleasant sensations;
- What is their intensity and duration;
- which provokes their strengthening;
- which helps to cope with pain.
Important!Be sure to tell the doctor how long you are concerned about such complaints, and whether you received any treatment earlier.

During a clinical inspection, the specialist evaluates:
- the position of the patient’s body, his gait, the volume of active and passive movements;
- the presence of skin defects, redness, peeling;
- symmetry of healthy and sick parts of the body;
- the presence of muscle spasm;
- the area of irradiation of pain;
- The presence of pain, temperature and other types of sensitivity.
During radiography, each spine for better visualization is studied individually.Pictures are performed in direct, lateral and (according to indications) of two oblique projections.To assess the stage and severity of degenerative-dystrophic changes, the X-ray classification of osteochondrosis of the spine of the zeaker is used.
Table: X -ray stages of osteochondrosis of the spine:
| Stage | Description |
| I (+) | Unexpressed changes in lordosis in a small number of segments |
| II (++) |
|
| III (+++) | Expressed changes, significant narrowing of the intervertebral holes |
| IV (++++) | Significant narrowing of the intervertebral holes, massive exostosis, often irreversible changes |

With insufficient information content of the R-picture, the patient can be prescribed more modern tests-CT (targeted images of one or more segments of the spinal column) and MRI (visual diagnostic method based on the properties of electromagnetic radiation).
Treatment
First of all, the doctor explains to the patient what osteochondrosis is and how to treat it.He talks about a set of measures that must be performed for a long period.
Therapy of the disease is carried out taking into account the stage.In the initial period of the disease, massage, physiotherapy, physiotherapy exercises are indicated.But as the dystrophic process progresses, various orthopedic devices for immobilizing the spine should be used.Drug treatment is also necessary.
Surgical intervention is indicated with complications and with the ineffectiveness of conservative treatment.
Medicines
The most important tasks of treatment with pharmacological drugs are the relief of pain, eliminating inflammation of nerve roots, restoring the structurality of cartilage, improving blood circulation and nutrition, stopping the development of pathology.There are several groups of drugs that can be prescribed in this case.
In pharmacies, they are represented in various forms and in a wide variety.The price of medicines can be different and you can always choose the most affordable.
Table No. 2.Medicines used in conservative therapy of osteochondrosis:
| Pharmacological group | Therapeutic effect | Instructions for use |
| Chondroprotectors | Slow down the processes of degeneration of cartilage, contributes to its restoration. | Take 1 capsule for a month.If necessary, the course of treatment is repeated. |
| NSAID | It has an anesthetic effect, reduces the inflammatory process. | Take on a tablet for pain.With severe pain, intramuscular injections of the drug are used. |
| B vitamins | Improves the conductivity of the nerve impulse, restores microcirculation in the area of the affected cartilage. | The course of treatment with intramuscular injections is carried out. |
| Musorelaxants | Relaxes muscles, relieves tension, facilitates pain. | Take one tablet 2 times a day. |
Drugs are prescribed according to the doctor’s testimony.Self -medication can be ineffective, and in some cases even harm.
Physiotherapy for osteochondrosis
What to do with osteochondrosis, except for medication, to accelerate recovery?One of the most effective methods of treating this disease is physiotherapy.
Its advantage is a selective effect on the focus of the disease.Physiotherapy contributions to reduce pain, elimination of inflammation, and increase general immunity.With their help, muscles relax, metabolic processes and blood circulation are normalized.
For osteochondrosis, they are successfully used:
- magnetotherapy;
- laser therapy;
- shock-wave therapy;
- quartz;
- electrophoresis;
- The effect of low frequency electric currents.
Physiotherapy do not carry out if the patient is in serious condition, with an exacerbation of the disease, oncological diseases, and mental disorders.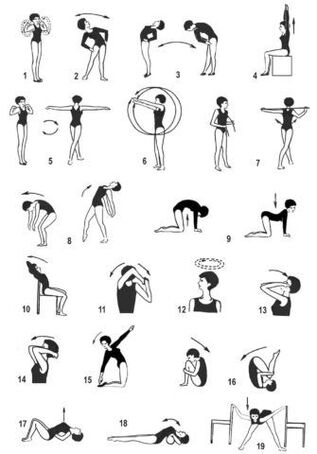 In other cases, physiotherapy has a beneficial effect on the recovery process, enhances the effect of drugs, which reduces their dosage.
In other cases, physiotherapy has a beneficial effect on the recovery process, enhances the effect of drugs, which reduces their dosage.
Medical physical education
Physical education classes are prohibited in the acute period of the disease.After eliminating this period, the doctor prescribes therapeutic exercises, which he develops together with the instructor individually for each patient.
With the help of exercises, the muscle corset is strengthened, which prevents the curvature of the spine and allows you to correctly and evenly distribute the load on the vertebrae.With regular physical exertion, medicinal substances penetrate the spine in higher concentrations than in their absence.
It is necessary to engage in the guidance of an experienced instructor and carefully monitor their condition.With discomfort and severe pain, the exercise should be stopped.
Prevention
Knowing what osteochondrosis is and its consequences, it will be useful to think about prevention.
Preventive measures are quite simple, they are easy to perform to everyone who cares about their health:
- prevention of injuries;
- regular physical training (swimming is very useful);
- maintain normal weight;
- Do not load the spine;
- monitor the correctness of posture;
- not to be in one position for a long time;
- Avoid sudden movements when lifting weights.
When fulfilling these rules, the period of remission will be long.
Osteochondrosis is a rather serious disease.But with timely seeking a doctor and adequate treatment, it is possible to stop its destructive effect.
Questions to the doctor
Pain in the neck
Hello, tell me please.I am 24 years old.For the past couple of months, the pain in the neck, the back of the head (sometimes still gives to whiskey, eyes).I also notice a strong crunch in the neck, tingling and numbness of hands, tongue, and sky.
I suspect osteochondrosis, becauseBoth mom and grandmother from youth are tormented with similar symptoms.Where to start the examination?And another question: can I go to aerobics?
Make an R-scheme (CT) Shop and Doppler of the vessels of the head and neck.You probably developed the vertebral artery syndrome against the background of cervical osteochondrosis.A further plan for diagnosis and treatment can be drawn up only after obtaining the results of these tests.
It is better not to visit aerobics yet.
Lumbar osteochondrosis
For seven years I have been tormented with the lower back, the exacerbation of osteochondrosis is almost every 2-3 months.Injections and tablets help for a short time, and then the pain returns.I work as a postman, it becomes harder.Are I put disability?
Hello!The decision on the award of the disability group is made by the ITU on the basis of a comprehensive study of your situation.First you need to contact the therapist and undergo an examination.
As a rule, with lumbar osteochondrosis, a disability group is not shown.Its award is possible with the development of complications (protrusions, intervertebral hernias, etc.).But, again, I repeat, everything is individual here.

























